Project Leader: Jill Taylor, PhD, LCSW | [email protected] | 314-353-5190 ext. 3102
Hospitalizations are costly for everyone. Disjointed transitions of care result in repeat, costly hospitalizations and poor health outcomes including death. Healthcare without the context of social and structural determinants of health (SSDOH) is ineffective and puts everyone at risk. FCHC Community Health Workers (CHW) and IHN Community Referral Coordinators (CRC) are experts in collecting data about patients’ experiences with SSDOH. When CHWs and CRCs are embedded in patient care and hospital settings focusing on partnership development and communication among respective teams, they can create change to improve transitions of care and help reduce costs.
YEAR 1 (2020) – PARTNERSHIP DEVEOPMENT
FCHC and partners collaborate to define roles, responsibilities and goals. Teams are flexible and adapt from original design due to COVID-19 pandemic. Hospital-based CRCs are essential to the plan.
CHWs Elicit Valuable Information about Root Cause
During the course of CHW’s work with patients during this project, a number of FCHC patients reported to CHW their hospital contact was related to being unhoused or experiencing substandard housing. Patients expressed the survival skill of “Three Hots and a Cot” (aka three meals and a bed) to CHW as motivating factors to seek out the hospital to meet their basic needs. Furthermore, a few patients during the project period expressed family dynamics and unstable relationships in their homes as contributing factors to hospitalizations. As CHW develops ongoing relationships with patients, they share more about the root cause for their expensive hospital encounters. This relationship between CHW and patients takes time to foster and holds key information that health care team members can take action to support patients with their needs.
Y1 Successes
1) No show rate at primary care post-hospitalization improved by 11%.
2) CHW completed PRAPARE with each patient who met criteria for high utilization.
3) CHW averaged 27 contacts with patients to coordinate care.
Lessons Learned to Share with Other Hospitals and Health Centers
-
-
- Interconnectedness of hospital and health center systems is key to creating change in transitions of care, which improves health outcomes, quality of life, and reduces health care costs. All too often, a safety net does not have all of the parts to bear the weight of patients’ social determinants of health.
- Community-based services (e.g. CHWs, community-based CRCs) are essential for understanding patients’ experiences and outreach to engage those who are otherwise unreachable.
- Build infrastructure for teams to have time and space to work together with the right players involved. CRCs and CHWs are uniquely positioned to access patients’ experiences and respond in a culturally-sensitive approach.
-
YEAR 2 (2021) – PARTNERSHIP EVOLUTION
Partnerships expanded to include SLU Family Medicine Residents and Diversity, Equity, and Inclusion Consultant to place an emphasis on health equity.
Patient-Centered Experiences
FCHC Community Health team developed a survey and sought feedback from FCHC MO HealthNet patients who have been hospitalized at St. Mary’s Hospital and are identified as frequent utilizers of the emergency room and hospital. Thirty-four (34) patients responded to the survey.
Survey questions (below) written with consideration of varying health literacy levels and validated by CHWs.
-
-
- Do you know you have MO HealthNet (also known as Medicaid) as your health insurance?
- If you receive MO HealthNet (aka Medicaid), what do you like about your insurance?
- What would you improve about your insurance?
- When you get medical care outside of FCHC (hospital, urgent care), what was the main reason you went there?
- When you get medical care outside of Family Care, do your doctors talk to each other to help you?
- What would you recommend your doctors do to improve their communication with each other to help you?
- Do you know that MO HealthNet (Medicaid) has a transportation option for you to go to medical appointments?
- Please circle the way(s) you usually get to and from your medical appointments.
- How reliable is your transportation? Please rate on a scale of 1-5.
- Have you ever gone to the hospital because you had nowhere else to go?
- Do your doctors understand what your life is like at home and in the community?
- Have you ever worked with a CHW at FCHC?
- Are there any resources or activities that you would like to see FCHC offer?
-
Themes of Patient Responses
1. Two of 34 patients did not know they had MO HealthNet.
2. Overall, patients reported appreciation for no out of pocket expenses and having access to their doctors. Two patients said, “Love it” in regard to their MO HealthNet coverage while a third patient stated, “Has been so much help to me with taking care of medical problems, my hospital bills, and taking care of me with all of that.”
3. While many of the patients said they would not change anything about their MO HealthNet coverage, a few patients stated they would improve “dental and optical” coverage for adults.
4. Reasons patients identified as needing to go somewhere other than FCHC to receive medical care involved: heart-related issues, kidneys, seizures, cancer, and “emergencies.” “Severe pain,” “pain management for my back and hip,” and “pain” were cited as reasons by 3 patients. Two patients stated, “Just if the clinic is closed” and “Family Care was closed or I couldn’t reach someone right away” when asked about their reasons for going to urgent care or the hospital.
5. 30 of 34 patients reported they believe their doctors talk to one another when they receive medical care outside of FCHC. Most patients followed up by giving credit to their primary care physicians for being “on top of it.” Most patients did not expand on how they know their doctors coordinate care.
6. Several patients either reported their “doctor is awesome” or reported they wanted their doctors talk to one another about medication when multiple doctors are involved in prescribing.
7. 28 of 34 patients know about the MO HealthNet transportation benefit. Five of the thirty-four patients reported they use the transportation benefit. One patient stated, “Always too slow I don’t like sitting and waiting; they left me at my appt.”
8. 26 of 34 patients stated they typically get to and from their appointments by car (either their own or someone else’s car).
9. Reliability of transportation was rated 4.38 out of 5 whether patients get to and from their appointments by car, MO HealthNet funded transportation, walking, cycling, Lyft, or taxi.
10. 6 of 34 patients reported they have gone to the hospital for care when they perceived they have not had anywhere else to go. One patient stated she went to the hospital, “when I was getting out of a domestic violence situation.”
11. 13 of 34 patients reported with certainty or ambivalence that their doctors do not understand what their life is like in their home and in the community. One patient stated, “they don’t understand how much of a struggle it is.” Another patient stated, “No, I don’t know. I don’t wish for anyone to be in my pain. If they lived with this pain I think they would understand better. I can barely deal with it sometimes. The pain is too much at one time. Plus Covid. If you could feel what I felt… lets find a cure! Another patient stated, “No, not really, they [doctor] don’t really talk about it. [CHW] is the only one that has taken the time to see what it is like.”
12. 15 of 34 patients recognized the title of Community Health Worker with whom they had worked with in the previous year despite each of them having connection with a CHW on more than one occasion.
13. Most patients did not have any suggestions for resources or activities that they would like to FCHC offer in the future. The common theme presented by a few patients was to provide more dental services for adults.
Y2 Successes
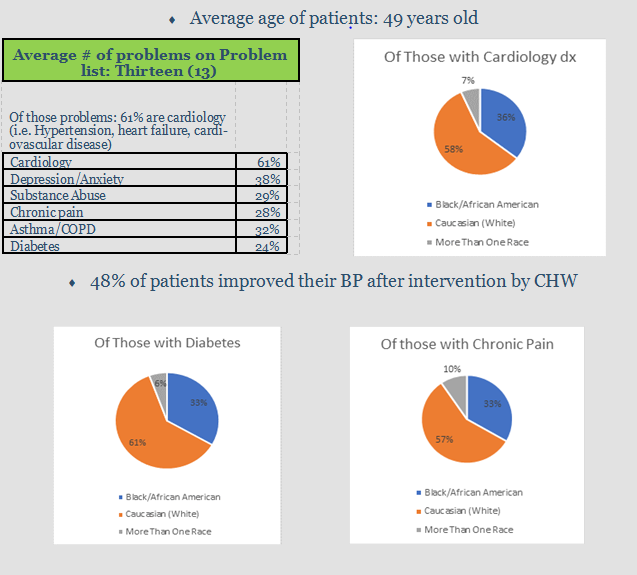
1) 48% of patients improved blood pressure reading after engagement by CHW and intervention by team members.
2) Workflow improvement.
3) Surveyed patients about their experiences with transitions of care.
Lessons Learned to Share with Other Hospitals and Health Centers
-
-
- Average number of Community Health Worker contacts per patient = 9 with some patients’ number of contacts reaching as high as 40.
- Community Health Workers often had to try to reach patients many times before a successful contact of reaching the patient. 37% of attempts to contact patients were unsuccessful while 63% of attempts to contact were successful. The relentless effort on the part of CHWs including outreach in the community by going to patients’ homes to knock on doors, leave notes, and leave basic necessities as an engagement tool is priceless in the process of reaching individuals who are otherwise unable to be reached. CHWs continued to engage in these activities during the pandemic and were able to connect patients to their care teams.
- Community Health Workers were, at times, the first to learn about a patient’s contact with the hospital system. CHWs developed a process to notify care team members.
- Relationship with Saint Louis University Family Medicine Residency further developed during the pandemic. A new strategy included second year residents shadowing Community Health Workers during a 4-week rotation, which put CHWs and residents in the same space to partner and develop real-time notification processes of all FCHC patients who were hospitalized at St. Mary’s Hospital. The real-time notification resulted in new workflows of CHWs assigned to this project notifying Community Health Team Leader about non-high utilizer patients’ hospitalizations. Subsequently, Community Health Team Leader requested other Community Health Workers on the team to follow up to screen and address SDOH. The intentional approach to connect with all FCHC patients who experienced emergency room and inpatient hospitalizations was to prevent future avoidable hospital system contact for social reasons.
- Community health team was more intentional about partnering with the FCHC behavioral health team throughout the grant period to address many patients’ significant behavioral health needs.
-
YEAR 3 (2022) – PARTNERSHIP EVOLUTION
Workflows hardwired among partners. Strong collaboration and data-informed mutual decision-making moved the project from concept to patient-centered quality in action.
Partnership Highlights
A number of connections with both our internal and external care partners have formed and developed throughout the duration of the Partnership project. The focus remained to improve understanding about their roles, the importance of collaboration, and to create changes to the benefit to the patient. The partnership highlights mentioned in this section are those that were key to a successful third year in this project.
Saint Louis Integrated Health Network Community Referral Coordinator
Coordination of care and consultation for barriers FCHC faced when navigating communication with hospital systems. The communication between CHWs and CRCs and our teams routinely meeting to discuss individual and collective experiences was critical to the success of this Partnership project.
Family Care Health Centers’ Pharmacy
Community Health Workers work alongside providers and pharmacists to problem-solve access to medication and health literacy. CHWs assisted with communication between patients and care team members related to medication to facilitate a quick, thoughtful resolution.
Family Care Health Centers’ Behavioral Health
Referrals for same-day consultation, psychiatry services, recovery support program, and Step Forward.
Family Care Health Centers’ Quality and Innovation team
Continually reviewed data points and provided information to the Community Health team for planning interventions (e.g. COVID vaccines, utilization of internal and external services).
Family Care Health Centers’ Nutrition Services
Sme day consultation and referrals for education and coaching.
Southern Illinois University Edwardsville School of Pharmacy
Under the direction of Kelly Gable, PharmD, BCPP, and Psychiatric Provider at Family Care Health Centers, SIUE Pharmacy Students completed medication reviews for MO Healthnet members post-hospitalization. They reviewed the results during weekly meetings with FCHC care team members to discuss findings and workflows to distribute and act on the information.
SLU Family Medicine Residency
1) PGY-2 Residents shadow Community Health Workers for their Community Medicine rotation to learn about SDOH and CHW workflows; 2) SLU Residency Faculty and Community Health team developed structure and workflows for Residents to pair with a CHW to conduct home visits for MO Healthnet members. The focus during the Partnership project was to visit patients who frequent the ED or admitted to the hospital and required a bridge appointment prior to coming into the health center for follow-up. These services will continue, as patients provided positive feedback about the combination of medical services combined with screening and referrals for SDOH.
Y3 Successes
1) SLU Family Med Residents join CHWs on home visits to improve patient care and experiences.
2) SIUE PharmD Students join the team to provide concise reports for care management and pre-visit planning that enhanced the work of the care team.
3) Patients who were deemed as having high utilization of hospital were tracked each year; only 13% of patients had high utilization in Y3 compared to Y1 after FCHC and partners’ interventions.
Transportation
Access to care is an issue that has many forms including but not limited to: insurance, location, cultural responsiveness, transportation, and health literacy.
Transportation is a social determinant of health and one point of access to care that presented as a barrier to many MO Healthnet members throughout the Partnership project. Community Health Workers screen patients’ social determinants of health utilizing PRAPARE (Protocol for Responding to and Assessing Patients Assets, Risks, and Experiences). CHWs recognized that many patients and providers reported transportation was a barrier to primary care. One Community Health Worker focused on the Partnership project invested time and energy in learning the transportation systems as they were designed to work and then listening to patients, providers, and other FCHC team members express problems that had a significant impact on various systems. More than responding to individual issues, the Community Health Worker collected aggregate data to share and invite communication to address processes in the spirit of improving access to primary care. A full overview of processes and transportation issues identified by Family Care Health Centers’ patients can be found here.
Memoriam
This report is dedicated to the memory of the seven patients who passed away during the third year of this grant project. The average age of the seven individuals who passed away was 49-years-old, and they lived with a variety of co-occurring chronic conditions. More importantly, they were individuals who had families, friends, neighbors, jobs, goals, and aspirations. Their lives matter, and their individual and collective experiences are central to the work the partners devote their efforts to evaluating and developing improved processes.
Health Equity
Health equity is the attainment of the highest level of health for all people, where everyone has a fair and just opportunity to attain optimal health regardless of race, ethnicity, disability, sexual orientation, gender identity, socioeconomic status, geography, preferred language, or other factors that affect access to care and health outcomes (CMS, 2022). We must look deeply into the ways our structures, policies, practices, norms, and values contribute to the ways inequities show up in our healthcare systems that perpetuate health outcomes that lead to vast differences in life expectancy based on the zip code one lives in the St. Louis region. Like African Americans throughout the U.S., Black residents of the St. Louis area are disproportionately affected by heart disease, high blood pressure, and infectious diseases. “The under-use and overuse of prescriptions,” are also Black community health concerns, according to Marcus Howard, the founder of GreaterHealth & Wellness, a culture-focused pharmacy start-up (Reid, 2021).
Community Health Workers are a necessary part of health equity work. CHWs identify issues, initiate culturally responsive conversations, and change systems to address injustices in various systems. Health systems must invest in culturally responsive, trauma-informed care approaches to addressing social and structural determinants of health to lay a foundation for healing-centered engagement and equitable care.
YEAR 4 (2023) – PARTNERSHIP EVOLUTION
Experience by providers – no turning back now! CHW’s are an essential member of the health care team and core to achieving health equity.
Partnership Highlights
-
-
- The objectives of this partnership project :
-
- Reduce avoidable hospitalizations for MO Healthnet recipients who frequent the ED and hospital
- Utilize partnerships to enhance communication and transitions of care to improve health outcomes through a health equity lens
- CHWs and CRCs screen and address SDOH and coordinate care among systems
- CHWs engage MO Healthnet recipients in primary care setting
- Provide safety net of care when patients experience barriers across systems
-
- Hospitalizations are costly – not only for the state and health care systems but also for individuals, families, and communities.
- Costs of hospitalizations for individuals include: lost time with family and pets, loss of income from time spent away from work, new medical bills, new supplies required at home, additional co-pays, loss of functioning and/or time to care for illnesses, and for some, loss of life.
- Our partners have mutual interests to reduce avoidable hospitalizations with MO Healthnet recipients’ experiences in the center of our work.
- The objectives of this partnership project :
-
Y4 Successes
1) SLU Family Medicine Residents present model of partnering with CHWs to Society for Teaching Family Medicine.
2) Address macro level social issues such as housing and transportation through advocacy.
-
-
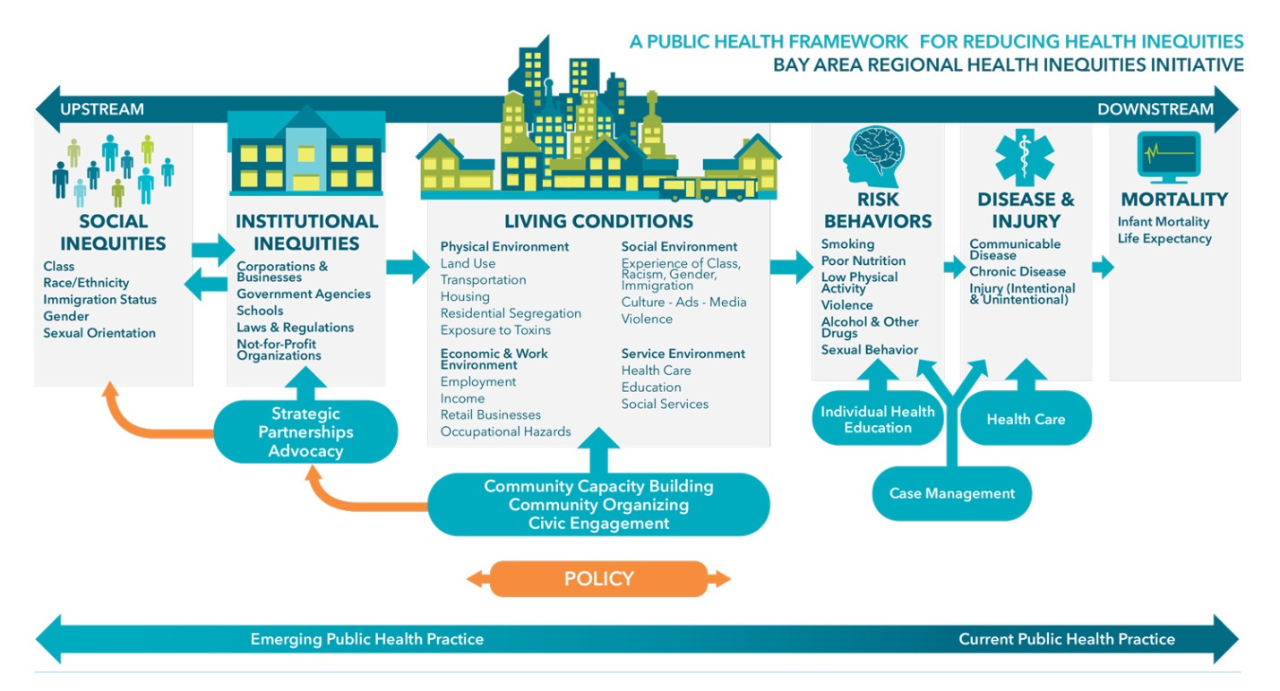
- Bay Area Regional Health Inequities Initiative infographic above represents our population health approach in this project.
- Partners identified the need to move from interventions at the disease & injury, risk behaviors, and living conditions levels to simultaneously addressing institutional inequities and social inequities.
- During monthly meetings and in between, CHWs and CRCs routinely identified and discussed social inequities of individual patients and the population. Furthermore, the team discussed strategies to address policy and structural change.
- Partnership relationships further developed to strengthen collective assets, abilities, and resources to address institutional inequities.
- Multi-aim approaches are necessary to effect change.
- CHWs and CRCs develop trust with patients and systems.
- Community Health Workers at Family Care utilize PRAPARE as a screening tool to understand individual and family systems’ SDOH.
- The population of patients at Family Care Health Centers who are identified as having high utilization of the ED and hospital average 4.2 SDOH.
- SDOH data informs the medical care team through CHWs’ documentation of patients’ assets, risks, and experiences.
-
Lessons Learned to Share with Other Hospitals and Health Centers
-
-
- Our work is collective, intentional, and unflinching to serve MO Healthnet recipients in under-resourced communities.
- Community Health Workers and Community Referral Coordinators emphasize humanistic approaches to health equity and healing centered engagement in health care.
- Relationships matter: CHWs and CRCs focus on relationships to set the stage to do their work.
- CHWs and CRCs meet MO Healthnet recipients in the community and in their homes, which facilitates engagement in unique ways that are unmatched by other professionals who engage in care coordination.
- Communication among systems requires resources, coordination, historical knowledge, and culturally responsive viewpoints.
- Understanding patients’ assets, risks, experiences helps to individualize and maximize benefit of care plans that promote shared decision-making.
- Commitment to work towards a value-based system of health care that yields equitable care is required.
-
Dedicated, knowledgeable partners work together to evaluate and address gaps in communication of multiple complex systems. Partnership development takes time and effort to yield results. Creating time and space to continually review processes and communication is essential. Sustainable funding for CHWs is necessary to respond to the social and structural determinants of health of MO Healthnet members.
NOTE:
Frequent utilization=3 ER visits, 2 inpatient visits, or 1 inpatient and 2 ER visits in a 12 month rolling period
“Community health workers are honestly my hero at FCHC. There are so many “I Wish” thoughts I have when it comes to my patients’ care. The CHWs have made some of those wishes a reality. By dropping off supplies for patients, helping them with rides to and from appointments, and checking in on what their needs are in general, they have made my job as a physician so much easier. All clinics, especially FQHCs, NEED appropriate funding for Community Health Workers.”
– Resident Physician at FCHC


QUOTES ABOUT COMMUNITY HEALTH WORKERS:
“Community Health Workers are so helpful! It feels really helpless to have a patient share a way in which they can’t be healthy because of a SDOH that is affecting their wellbeing such as housing insecurity or access to BP machines or healthy food– it’s such a gift to be able to ask a CHW to reach out to them to support the patient as a whole person.” – Registered Nurse at FCHC
“CHWs have elevated the voice of patients so that I am better able to empathize about what it is like to be one of our patients.” – Chief Behavioral Health Officer at FCHC
“The CHWs really put the Family in Family Care.” – Dentist at FCHC
[CHWs] “Bridging the gap between the patients and the providers.” -Primary care provider
